Home > Treatments > Female Infertility >
Isthmocele Repair
At Mamata Fertility Hospital in Secunderabad, we are dedicated to advancing women’s health through state-of-the-art treatments for complex gynecological and fertility conditions. Isthmocele Repair is one such innovative solution, offering relief for women impacted by cesarean scar defects (CSDs). With a personalized approach and minimally invasive methods, our expert team is committed to helping women regain their reproductive potential and improve their overall quality of life.
QUICK FACTS
- Hospital stay: Approx 1 day
- Anaesthesia: Local
- Covered by health insurance? Yes
- Procedure duration: ~20 minutes.
98% of our patients are likely to recommend us to their peers
Transparent & Empathetic Process
Comprehensive & Prompt Care
Internationally & nationally renowned consultants
For Appointment, Please Call:
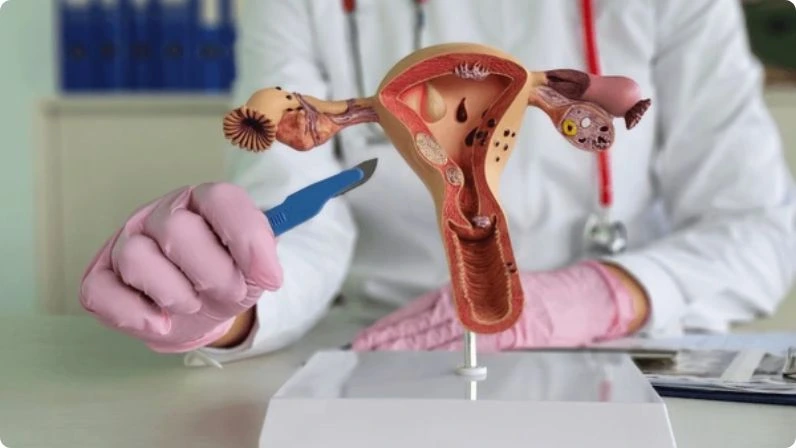
What is Isthmocele Repair?
Isthmocele repair is a surgical procedure designed to treat a cesarean scar defect (CSD), also known as a uterine isthmocele. An isthmocele is a small pouch or indentation that develops at the site of a previous cesarean incision in the uterus. This defect can cause irregular bleeding, pelvic pain, or challenges with fertility, as it disrupts the uterine environment.
At Mamata Fertility Hospital, we utilize advanced techniques like hysteroscopy or laparoscopy to repair the defect, restoring the uterine structure and function. This targeted treatment not only addresses symptoms but also enhances fertility outcomes for women trying to conceive.
Benefits of Isthmocele Repair
Treating an isthmocele through surgical repair offers numerous advantages for your health and reproductive goals. Here’s how it can help:
1. Restores Uterine Integrity
The repair procedure strengthens the integrity of the uterine wall, reducing the risks of complications in future pregnancies.
2. Eliminates Symptoms
Chronic symptoms like abnormal uterine bleeding, pelvic pain, and bloating often resolve after the defect is repaired.
3. Improves Fertility
By addressing the scar defect, the uterine cavity returns to its natural shape, facilitating better implantation and pregnancy outcomes.
4. Prevents Pregnancy Complications
Repairing the defect minimizes the risks of uterine rupture, placenta issues, and miscarriage in subsequent pregnancies.
5. Utilizes Minimally Invasive Surgery
Advanced techniques like hysteroscopic or laparoscopic repair ensure minimal discomfort, faster recovery, and reduced scarring.
Who Can Benefit from Isthmocele Repair?
Isthmocele repair in Secunderabad is a life-changing procedure for women who experience symptoms or fertility issues related to cesarean scar defects. You may benefit from this surgery if you have the following conditions:
- Abnormal Uterine Bleeding: Spotting or irregular bleeding after menstruation due to blood pooling in the defect.
- Chronic Pelvic Pain: Discomfort caused by inflammation or scar-related pressure.
- Secondary Infertility: Difficulty conceiving or recurrent miscarriages due to structural interference in the uterine cavity.
- Complications in Previous Pregnancy: Uterine rupture or placenta complications linked to a thin or weakened cesarean scar.
- Desire for Future Pregnancies: Women planning future pregnancies who need a strong and healthy uterine wall.
Our specialists at Mamata Fertility Hospital perform thorough evaluations using diagnostic tools like ultrasounds, hysteroscopy, or MRI to determine if istmocele repair is the right choice for your case.
What to Know Before Surgery?
Before undergoing isthmocele repair, it’s important to understand the procedure and your health implications. Here are key points to keep in mind:
1. Diagnosis is Crucial:
A cesarean scar defect can be confirmed through imaging tests like a sonohysterography or an MRI. Knowing the size and location of the defect helps in planning the surgery effectively.
2. Risks and Benefits:
Isthmocele repair is generally safe and effective, but like any surgery, it comes with minor risks such as infection or temporary discomfort. Our medical team takes every step to minimize potential complications.
3. Fertility Goals:
Discuss your fertility plans. Repairing the defect improves uterine health, increasing your chances of conception and reducing pregnancy risks.
4. Healing Timeline:
Depending on the type of surgery, complete healing may take 6-12 weeks. During this period, it is vital to follow the recovery guidelines for optimal results.
At Mamata Fertility Hospital, we prioritize patient education, ensuring you are fully informed and confident before your surgery.
How to Prepare for the Procedure?
Preparation plays a vital role in ensuring the success of your isthmocele repair surgery. Here’s how you can get ready for the procedure:
1. Medical Prep & Diagnostics:
- Undergo all recommended tests to evaluate your health and confirm the surgical plan.
- Disclose your medical history, especially any medications or conditions, to your doctor.
2. Stop Medications if Needed:
Certain medicines, especially blood thinners, might need to be paused before surgery. Follow your surgeon’s advice closely.
3. Make Lifestyle Adjustments:
- If you smoke, consider quitting before surgery as it can hinder healing.
- Maintain a balanced diet and stay hydrated to boost recovery.
4. Arrange for Post-Surgery Care:
- If required, ask a family member or friend to assist you for the first few post-surgery days.
- Make arrangements for child care or household help to allow yourself ample rest.
Our team at Mamata Fertility Hospital provides you with a personalized preparation checklist, ensuring you feel supported every step of the way.
The Isthmocele Repair Procedure
Isthmocele repair surgery is a tailored approach aimed at addressing the specific needs of each patient. Here’s an overview of the process:
1. Pre-Surgical Consultation and Diagnosis
- A detailed medical history is reviewed, and diagnostic imaging is used to pinpoint the size, location, and depth of the defect.
- Your specialist will discuss the most suitable repair technique based on your symptoms, fertility goals, and overall health.
2. Types of Isthmocele Repair Surgery
Hysteroscopic Repair
- Best for: Minor defects located within the uterine cavity.
- Approach: A tiny camera and surgical instruments are passed through the cervix to remove scar tissue and smooth the uterine lining.
Laparoscopic Repair
- Best for: Larger defects or those extending beyond the uterine cavity.
- Approach: Small incisions in the abdomen allow surgical tools to repair the defect and reinforce the uterine wall.
Combined Approach
- Best for: Complex cases requiring internal and external scar correction.
- Approach: A combination of hysteroscopy and laparoscopy ensures comprehensive repair.
3. Post-Repair Closure
After the defect is repaired, the uterine wall is reinforced to optimize strength and healing.
Our team at Mamata Fertility Hospital focuses on using minimally invasive methods whenever possible to ensure faster recovery and better outcomes for every patient.
Choosing the Right and Best Type of Repair for Your Case
Selecting the most appropriate method for isthmocele repair depends on factors such as the severity of the defect, your symptoms, and whether or not you are planning future pregnancies. Here’s an overview of options and how our specialists at Mamata Fertility Hospital determine the best choice for your case:
1. Hysteroscopic Repair
- Best For: Small defects localized within the uterine cavity.
- Ideal Candidates: Women with minimal symptoms seeking a minimally invasive solution, particularly those aiming for fertility restoration.
2. Laparoscopic Repair
- Best For: Larger defects or those extending deep into the uterine wall.
- Ideal Candidates: Women experiencing significant symptoms or at a higher risk for complications in future pregnancies.
3. Combined Repair Approach
- Best For: Complex, multiple-layer defects that require thorough correction.
- Ideal Candidates: Women needing a comprehensive solution to eliminate symptoms while enhancing uterine strength for future pregnancies.
At Mamata Fertility Hospital, diagnostic evaluations such as ultrasound, hysteroscopy, or MRI scans help us analyze your condition and recommend the best repair method tailored to your needs and goals.
Recovery and Aftercare
Recovery after isthmocele repair surgery depends on the type of procedure performed and individual factors. Here’s what to expect during the healing process:
Immediate Post-Surgery Care:
- Most patients can return home the same day or within 24 hours, especially for minimally invasive surgery.
- Pain and discomfort are typically mild and manageable with prescribed medications.
Healing Timeline:
- For hysteroscopic repair, most women are back to their daily activities within 1-2 weeks.
- For laparoscopic repair, full recovery may take 2-4 weeks.
Follow-Up Appointments:
Regular check-ups ensure proper healing and assess results. Imaging tests may be conducted to confirm the success of the repair.
At Mamata Fertility Hospital, we provide personalized aftercare plans, guiding you through every stage of recovery to ensure optimal health and well-being.
Success Rates
The success of isthmocele repair largely depends on the severity of the defect and your overall health. At Mamata Fertility Hospital, we are proud to offer high success rates for this procedure, supported by our expertise in advanced surgical care:
- Over 85% of women experience complete symptom resolution after istmocele repair.
- Fertility outcomes improve significantly, with most patients achieving successful pregnancies within a year.
- Long-term risks such as uterine rupture or complications in future pregnancies are greatly reduced.
Our focus on cutting-edge techniques ensures the best possible results for all our patients.
Isthmocele Repair and Future Pregnancies
One of the major benefits of isthmocele repair is its positive impact on future pregnancies. Here’s what you should know about how the procedure influences conception and childbirth:
1. Improved Fertility:
Repairing the cesarean scar defect restores the uterine cavity’s natural environment, ensuring better implantation and reducing miscarriage risks.
2. Lower Risk of Uterine Rupture:
A repaired uterine wall is significantly stronger, minimizing the chances of rupture during labor or subsequent pregnancies.
3. Better Placenta Attachment:
The surgery corrects scar-related irregularities, ensuring the placenta can attach securely and function properly for the full term of pregnancy.
4. Recommendations for Future Pregnancies:
- After isthmocele repair, conception is generally safe after 3-6 months, allowing enough time for healing.
- Discuss the safest delivery mode with your doctor. While VBAC (vaginal birth after cesarean) may be possible, C-sections are often recommended for extremely complex cases to reduce stress on the uterine wall.
At Mamata Fertility Hospital, we guide our patients through every stage of family planning after surgery to ensure safe and successful outcomes.
Cost of Isthmocele Repair in Secunderabad
At Mamata Fertility Hospital, we are committed to making high-quality care accessible. The cost of istmocele repair in Secunderabad can vary based on factors like the procedure type, diagnostic tests, and aftercare services. Here’s an approximate cost breakdown:
- Consultation and Diagnostic Tests: ₹8,000 – ₹12,000
- Hysteroscopic Repair: ₹50,000 – ₹80,000
- Laparoscopic Repair: ₹1,00,000 – ₹1,50,000
- Post-Surgery Follow-Up Care: Costs depend on individual requirements.
Our team will help you understand pricing details and assist with insurance coverage or payment plan options for your convenience.
Making an Informed Decision
Choosing to undergo isthmocele repair surgery is a significant step toward improved health and fertility. At Mamata Fertility Hospital in Secunderabad, we combine compassionate care, state-of-the-art techniques, and personalized treatment plans to help our patients achieve the best possible outcomes.
Next Steps:
- Schedule Your Consultation: Discuss your symptoms and goals with our experienced specialists.
- Understand Your Options: Learn about the surgical approaches and choose the procedure that meets your needs.
- Plan for Success: With expert guidance, start your healing and recovery journey confidently.
FAQs
1. How do I know if I have an isthmocele?
Symptoms such as abnormal bleeding, pelvic pain, or infertility may indicate an isthmocele. A specialist can confirm the diagnosis with an ultrasound or hysteroscopy.
2. Will this surgery improve my chances of getting pregnant?
Yes, repairing the defect restores the uterine cavity, increasing the likelihood of natural conception and reducing the risks of pregnancy complications.
3. Is istmocele repair safe?
Isthmocele repair is considered safe, especially when performed using minimally invasive techniques. The risks of complications are minimal, and most patients recover quickly.
4. Can scar defects reoccur after surgery?
While the procedure is highly effective, scar healing varies among individuals. Following your surgeon’s post-operative care advice minimizes the risk of recurrence.
5. How long should I wait to try for a pregnancy after surgery?
It’s generally recommended to wait 3-6 months to allow the uterus to fully heal before attempting conception.
We Can Help You With All The Possible Infertility Treatments.
WHAT PATIENTS EXPERIENCE AT MAMATA FERTILITY?
“I had an excellent first visit to Mamata Hospitals, where I met Dr. Mamata madam and Dr. Arti. Madam and Dr cheatn The process was systematic, instilling confidence that my issues will be effectively addressed. The staff and doctors were incredibly friendly and supportive, making me feel at ease. Their professionalism and warmth have given me great confidence in their care. I look forward to sharing more about my journey in detail.”
Vishu S.N
At Mamata Fertility Hospital, we combine surgical expertise, advanced technology, and compassionate care to ensure successful outcomes for fibroid removal surgery. Whether you’re planning for pregnancy or need relief from symptoms, our team is here to guide you every step of the way. Contact us today to schedule a consultation and start your personalized treatment plan!

Dr Aarti Deenadayal Tolani
MBBS, MS ( OBGYN), FICOG
Clinical Director, Scientific In- Charge & Fertility Consultant with 15+ years Of Experience

